Algorithms, Clinical Research & Data, Escalation Therapy, Hemodynamics
Managing Patients with Short-Term Mechanical Circulatory Support
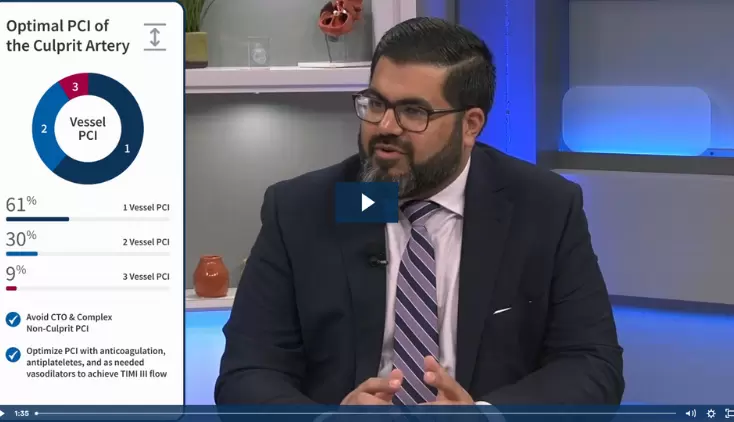
Tim Balthazar, MD, discusses his recent paper “Managing Patients with Short-Term Mechanical Circulatory Support: JACC Review Topic of the Week.” The paper describes practical approaches to optimizing care for patients with cardiogenic shock supported with an Impella® heart pump. Dr. Balthazar, a cardiologist and intensivist at University Hospital in Brussels, Belgium, discusses device timing and selection, device positioning, and escalation decisions.
Regarding device timing and selection, Dr. Balthazar explains that choosing which device you need depends on when you start support and how much flow you need at that point. “Don’t wait too long,” he emphasizes, “because the longer you wait, the more flow you will need to reverse the shock stage, especially because the microcirculation will fail. You will get production of NO and you will get vasoplegia and it will be a lot more difficult to reverse the shock.”
Dr. Balthazar discusses figures 1 and 2 in paper showing the benefits of starting pVAD support at SCAI shock stages C and D. He notes, however, “I think the most important question is not exactly which stage… You’re a clinician. You should take the context and look at what you expect from the evolution more than only the shock stages… I’m not sure if, really, black and white usage of these criteria is the way to go. I mean, if it’s a really bad situation, probably Stage B could be considered as well to start with Impella.”
Regarding device positioning, Dr. Balthazar explains, “I keep hearing about hemolysis, and to be honest, in my personal experience it’s rare to see severe hemolysis. But it’s almost always, it has to do something with suction. And suction, in a lot of cases, has to do with positioning of the device.” He then describes tools to ensuring proper Impella position including daily chest x-rays and echocardiography.
Escalation is the topic that received the most interest in this review. Figure 5 presents an algorithm for approaching deteriorating hemodynamics during LV pVAD support. Benham Tehrani, MD, tweeted that this algorithm should be laminated and put in ICUs.
“In my mind its one of the most important parts of the paper,” Dr. Balthazar explains, “because I’ve seen how patients are escalated, for example to ECMO, because they think patients need escalation. And very often its just because the Impella is not performing optimally, or the context isn’t interpreted in the right way. So I think we should try to have a very structured approach to that.” Dr. Balthazar walks through the algorithm explaining decision points regarding pressure vs flow and reasons for insufficient flow. “If flow is insufficient, you should always ask yourself: Is this because the patient needs more flow than I can give with the device? Or is this because my device is just not working properly? That’s a crucial question.” As interviewer Seth Bilazarian, MD, notes, Impella can’t optimally serve the patient if it’s not being used optimally.
NPS-1938